HEALTH
'World first' for double hand transplant patient
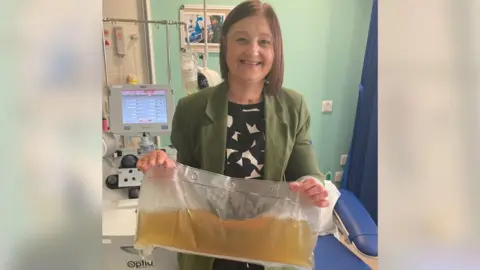
A woman who had a double hand transplant has undergone pioneering NHS treatment to prevent her body rejecting them.
Tanya Shepherd, from Hull, became the UK’s first female recipient of two replacement hands in 2018, only for her immune system to identify the tissue as foreign.
Now, in what is thought to be a world first, she has received a blood treatment called plasma exchange, in which antibodies are removed to reduce the risk of rejection.
Ms Shepherd, 48, said rejection was "a real and scary risk", but she was "honoured" to be the first to trial the treatment.
Her symptoms, which included swelling, reduced dexterity and changes in skin pigmentation, have now begun to improve.
Ms Shepherd received a double hand and arm transplant at Leeds General Infirmary in September 2018 after losing both hands and three-quarters of her left arm to sepsis.
However, she began suffering symptoms of antibody mediated rejection (AMR) – a type of rejection where the immune system identifies the tissue as foreign and produces antibodies to fight it.
She is being treated in Leeds by Therapeutic Apheresis Services, an NHS team which removes harmful, disease-forming proteins, chemicals or cells from patients' blood.
Ms Shepherd has received 10 sessions of therapeutic plasma exchange, in which plasma is removed from the blood to quickly decrease or remove the antibodies.
She is now due to begin immunosuppressive treatment in the hope of preventing antibody levels from rising again.

Dr James Griffin, a medical director at NHS Blood and Transplant, said: “Our aim is to protect the transplant while other therapies work to stop Tanya’s immune system from making the antibodies and we’re pleased that the treatment has served to ease Tanya’s symptoms.”
Ms Shepherd said the treatment had been made possible by "generous blood and plasma donors" and urged more people to sign up.
"I’m eternally grateful to those who already have, who have helped me on my journey,” she added.
Health minister Andrea Leadsom said: "Organ rejection is a real risk for transplant recipients and can have devastating consequences.
“NHS Blood and Transplant continues to champion innovative treatments like this world first plasma exchange, allowing people to receive further treatment and live their lives to the fullest.”
Richard Scolyer: Top doctor remains brain cancer-free after a year

A year after undergoing a world-first treatment for glioblastoma, Australian doctor Richard Scolyer remains cancer-free.
The esteemed pathologist's experimental therapy is based on his own pioneering research on melanoma.
Prof Scolyer's subtype of glioblastoma is so aggressive most patients survive less than a year.
But on Tuesday the 57-year-old announced his latest MRI scan had again showed no recurrence of the tumour.
"To be honest, I was more nervous than I have been for any previous scan," he told the BBC.
"I'm just thrilled and delighted... couldn't be happier."
Prof Scolyer is one of the country's most respected medical minds, and was this year named Australian of the Year alongside his colleague and friend Georgina Long, in recognition of their life-changing work on melanoma.
As co-directors of the Melanoma Institute Australia, over the past decade the pair's research on immunotherapy, which uses the body's immune system to attack cancer cells, has dramatically improved outcomes for advanced melanoma patients globally. Half are now essentially cured, up from less than 10%.
It's that research that Prof Long, alongside a team of doctors, is using to treat Prof Scolyer - in the hope of finding a cure for his cancer too.
In melanoma, Prof Long - herself a renowned medical oncologist - and her team discovered that immunotherapy works better when a combination of drugs is used, and when they are administered before any surgery to remove a tumour. And so, Prof Scolyer last year became the first brain cancer patient to ever have combination, pre-surgery immunotherapy.
He is also the first to be administered a vaccine personalised to his tumour's characteristics, which boosts the cancer-detecting powers of the drugs.
After a tough couple of months of treatment at the start of the year - spent dealing with epileptic seizures, liver issues and pneumonia - Prof Scolyer says he is feeling healthier.
"I'm the best I have felt for yonks," he said, adding that he's back to exercising every day - which for him often means a casual 15km (9.3 mile) jog.
"It certainly doesn't mean that my brain cancer is cured... but it's just nice to know that it hasn't come back yet, so I've still got some more time to enjoy my life with my wife Katie and my three wonderful kids."
The results so far have generated huge excitement that the duo may be on the cusp of a discovery which could one day help the roughly 300,000 people diagnosed with brain cancer globally each year.
Prof Scolyer and Prof Long have previously said the odds of a cure are "minuscule", but they hope the experimental treatment will prolong Prof Scolyer's life and will soon translate into clinical trials for glioblastoma patients.
They currently have a scientific paper under review, which details results from the first weeks of Prof Scolyer's treatment, but Prof Long stresses that they are still a long way off developing an approved and regulated course of treatment.
"We've generated a whole heap of data, to then make a foundation for that next step, so that we can help more people," she said.
"We're not there yet. What we have to really focus on is showing that this pre-surgery, combination immunotherapy type of approach works in a large number of people."
Roger Stupp - the doctor after whom the current protocol for treating glioblastomas is named - earlier this year told the BBC Prof Scolyer's prognosis was "grim", and that it was too early to tell if the treatment is working.
He added that while Mr Scolyer's earlier results were "encouraging", he wanted to see him reach 12 months, even 18, without recurrence before getting excited.
Prof Scoyler said he's already proud of the data his treatment has generated and grateful to his family and his medical team for supporting "this experiment".
"I feel proud of the team that I work with. I feel proud that they're willing to take the risk in going down this path."
"[It] provides some hope that maybe this is a direction that's worth investigating more formally."